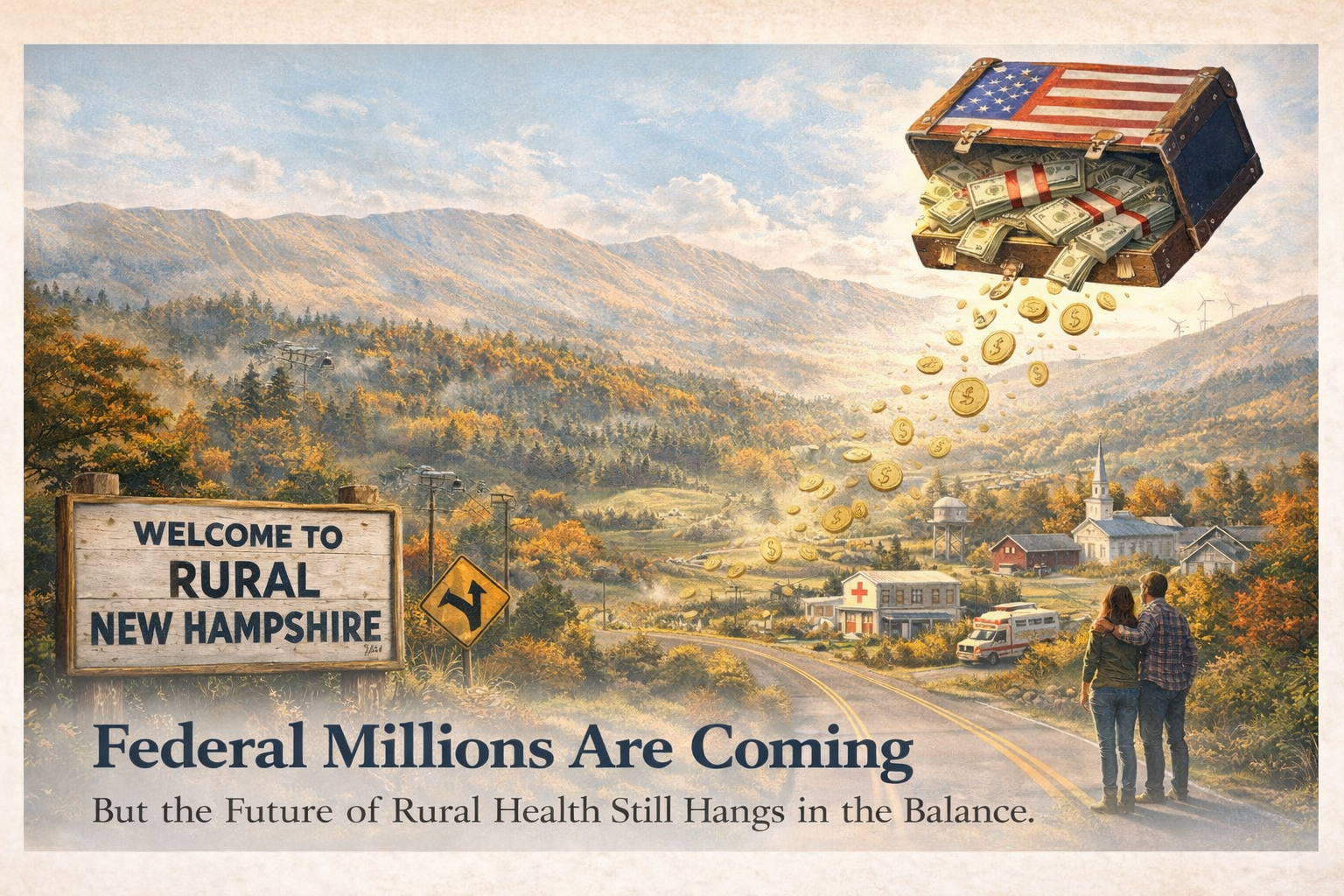
Federal Millions Are Coming But the Future of Rural Health Still Hangs in the Balance
New Hampshire is at a pivotal moment for rural health care—one that brings both new opportunity and renewed responsibility.
Governor Kelly Ayotte recently announced that New Hampshire has been awarded $204 million in federal funding through the 2026 Rural Health Transformation Program, administered by the Centers for Medicare & Medicaid Services (CMS). It is the largest award among all New England states, and it positions New Hampshire to be a regional leader in reshaping rural health care delivery.
Over the next one to five years, the state will receive hundreds of millions more as part of a new $50 billion federal initiative designed to strengthen rural health systems across the country. The funding will be managed through a newly created entity—the Governor’s Office of New Opportunities & Rural Transformational Health (GO-NORTH)—with strategic goals that include preventive care and behavioral health, workforce development, innovative delivery models, and long-term sustainability.
This is significant. But it does not change the underlying reality: rural health care in New Hampshire remains fragile, particularly for communities that rely heavily on Medicaid and safety-net providers. This moment will only matter if the funding is deployed deliberately, transparently, and in close partnership with the rural communities most affected by long-standing access and affordability challenges.
What happens next is crucial, and here is why….
Our Rural Health Care System Is Under Strain
Nearly 47% of Granite Staters live in rural communities, where hospitals, clinics, and primary care practices operate with thin margins and limited staffing. These providers are often the sole source of emergency, primary, behavioral, and maternity care for large geographic regions. When they struggle—or close—the effects ripple far beyond health outcomes, weakening local economies and community resilience.
This new funding should arrive in New Hampshire in early 2026, during a state budget cycle in which the New Hampshire Department of Health and Human Services was already forced to cut $25.5 million, including reductions to at-home nurse visitation, elder care, and homelessness prevention. At the same time, federal Medicaid and ACA cuts are beginning to take effect, increasing premiums and out-of-pocket costs for New Hampshire families and businesses and threatening the financial stability of the very networks of care that this new funding is meant to sustain.
Recent events underscore how precarious the current situation remains. We have begun to see warning signs in rural New Hampshire with closures of the Franconia Health Center and the Health First Center in Canaan in 2025. For North Country residents, that means longer travel times, fewer choices, and delayed care. Similar pressures are being felt across rural New Hampshire.
What the New Funding Can—and Cannot—Do
CMS officials have been clear: this investment is not a bailout or an offset for existing losses or current cost pressures. The amount of funding that can be used to fund hospitals and other medical providers is capped at 15%. As CMS Administrator Mehmet Oz put it, the purpose of the $50 billion national program is to “right-size the system” and address the structural barriers that have allowed rural health outcomes to worsen over decades—not simply to pay off existing bills. States that fail to meet benchmarks or carry out promised reforms risk losing funds.
That makes New Hampshire’s next steps critical.
The state’s application—developed with input from more than 300 organizations and individuals—lays out a vision for modernizing rural health care through better payment models, stronger workforce pipelines, expanded behavioral health, and improved integration between primary care and public health. These goals align closely with findings from national research, including recent warnings that rural primary care in America is nearing a breaking point.
But vision alone is not enough. Implementation must be well-resourced and well-executed.
GO-NORTH is an independent unit of the Governor’s Office working with the New Hampshire Department of Health and Human Services to leverage DHHS infrastructure and expertise to support implementation of the program and advance innovative approaches to rural health care delivery. While the scale of this funding is unprecedented, so too are the demands it places on the system responsible for administering it. For DHHS and the newly created GO-NORTH office, managing hundreds of millions of dollars on accelerated timelines—across initiatives that are new, complex, and still being defined—will be a significant operational lift. It will be critical to establish clear governance, sufficient oversight capacity and transparent benchmarks at the outset, to ensure accountability for both the funding and the expected outcomes.
Rising Costs, Shrinking Options
Even as this funding offers hope, cost pressures continue to mount. The Kaiser Family Foundation reports that the sharp rise in ACA premiums in 2026 have presented many consumers with premium increases of 50–75% as insurers adjust to federal funding changes. For rural families, seasonal workers, and small business owners, these increases are pushing both care and coverage out of reach—driving more people into medical debt or forcing them to delay care until emergencies arise.
At the same time, Medicaid cuts from the 2025 One Big Beautiful Bill Act threaten to:
Accelerate rural hospital closures,
Reduce access to obstetrics, behavioral health, and primary care,
Shift costs onto families, employers, and local governments.
Hospitals and health clinics are not just care providers in rural New Hampshire—they are often major employers and economic anchors of community life. When they falter, entire regions feel the impact.
What Comes Next: Turning Investment Into Impact
This funding brings an opportunity to transform rural health for the next generation. While it also demands coordination, accountability, and sustained engagement.
The New Hampshire Health Cost Initiative is working with community stakeholders to advance these essential actions:
Strengthening primary care and community health networks
Invest in community health centers, mobile clinics, expanded pharmacy access and telehealth to bring care closer to where people live.
Elevating local voices
Nurses, EMS teams, pharmacists, patients, parents, and small business owners must shape how these funds are used. Solutions imposed from above will not have the same impact as solutions developed by those with local knowledge.
Advocating for smart, sustained investment
One-time funding cannot compensate for structural underfunding. Policymakers must understand that a healthy state is also an economically resilient one.
Building partnerships and innovation
Public health, providers, nonprofits, local governments, and the private sector must work together—through shared services, co-located care, and new delivery models.
A Moment That Matters
The $204 million award launches a once-in-a-generation opportunity. It signals confidence in New Hampshire’s readiness to lead. But it does not erase the risks facing rural health care—or the impact of underinvestment. And, it should not be seen as a way to mask the consequences of other harmful policy choices that were made in recent federal and state budgets.
Health care is the foundation of opportunity, economic stability, and quality of life in New Hampshire. If we get these investments right, rural communities can become stronger, more resilient, and better equipped to meet future challenges. If we don’t, the warning signs we’re seeing today will only multiply.
This is not the end of the story. It is a new chapter where strategic investment, community-based leadership and public accountability matter most.